Cryptococcosis in Cats and Dogs
Introduction
Cryptococcosis is caused by the C. neoformans – C. gattii complex comprised of 8 distinct genotypes (VNI – VNIV and VGI – VGIV). While incidence varies by geographic location, clinical manifestations are similar for all genotypes. Cryptococcosis occurs worldwide and is most common in the western U.S. and Canada and in Australia. Cryptococcus is found in soil and decaying matter. Soil contaminated with bird droppings, especially of pigeons, has been implicated in creating an ideal ecological niche for the growth of Cryptococcus [1Emmons CW. Saprophytic sources of Cryptococcus neoformans associated with the pigeon (Columba livia). American journal of hygiene 1955;62:227-232.]. Due to higher body temperature, birds rarely develop disease, but can shed Cryptococcus in feces, which can survive for years in the environment [1Emmons CW. Saprophytic sources of Cryptococcus neoformans associated with the pigeon (Columba livia). American journal of hygiene 1955;62:227-232.]. Infection is thought to occur when basidiospores (infective propagules) are aerosolized and inhaled. Not surprisingly, living within 10 km of significant soil disturbance or logging or partaking in outdoor activities such as hiking and visiting botanic gardens have all been shown to increase the risk of cryptococcosis in dogs and cats [2Duncan CG, Stephen C, Campbell J. Evaluation of risk factors for Cryptococcus gattii infection in dogs and cats. J Am Vet Med Assoc 2006;228:377-382.]. Ingestion and cutaneous inoculation have also been considered possible routes of infection but is likely much less common [3Malik R, Hunt GB, Bellenger CR, et al. Intra-abdominal cryptococcosis in two dogs. J Small Anim Pract 1999;40:387-391., 4Medleau L, Hall EJ, Goldschmidt MH, et al. Cutaneous cryptococcosis in three cats. J Am Vet Med Assoc 1985;187:169-170.]. Even cats confined to indoors are at risk, suggesting Cryptococcus is found in the home [5Trivedi SR, Sykes JE, Cannon MS, et al. Clinical features and epidemiology of cryptococcosis in cats and dogs in California: 93 cases (1988-2010). J Am Vet Med Assoc 2011;239:357-369., 6Gerds-Grogan S, Dayrell-Hart B. Feline cryptococcosis: a retrospective evaluation. J Am Anim Hosp Assoc 1997;33:118-122.].
Signalment
Cryptococcosis is at least 5 and 3 times more likely in cats than in dogs and horses, respectively [7McGill S, Malik R, Saul N, et al. Cryptococcosis in domestic animals in Western Australia: a retrospective study from 1995-2006. Medical mycology 2009;47:625-639.]. Any aged animal can be affected and average age is 6-8 years for cats and 2-3 years for dogs [5Trivedi SR, Sykes JE, Cannon MS, et al. Clinical features and epidemiology of cryptococcosis in cats and dogs in California: 93 cases (1988-2010). J Am Vet Med Assoc 2011;239:357-369., 6Gerds-Grogan S, Dayrell-Hart B. Feline cryptococcosis: a retrospective evaluation. J Am Anim Hosp Assoc 1997;33:118-122., 7McGill S, Malik R, Saul N, et al. Cryptococcosis in domestic animals in Western Australia: a retrospective study from 1995-2006. Medical mycology 2009;47:625-639., 8O’Brien CR, Krockenberger MB, Martin P, et al. Long-term outcome of therapy for 59 cats and 11 dogs with cryptococcosis. Aust Vet J 2006;84:384-392., 9Malik R, Wigney DI, Muir DB, et al. Cryptococcosis in cats: clinical and mycological assessment of 29 cases and evaluation of treatment using orally administered fluconazole. J Med Vet Mycol 1992;30:133-144.]. In general the age distribution in dogs is primarily younger in contrast to cats which have a much wider age distribution. Breed and sex predilections have been inconsistent between studies. Some have shown a predisposition for pure bred cats such as the Abyssinian, Birman, Siamese, and Ragdoll and others have not [7McGill S, Malik R, Saul N, et al. Cryptococcosis in domestic animals in Western Australia: a retrospective study from 1995-2006. Medical mycology 2009;47:625-639., 9Malik R, Wigney DI, Muir DB, et al. Cryptococcosis in cats: clinical and mycological assessment of 29 cases and evaluation of treatment using orally administered fluconazole. J Med Vet Mycol 1992;30:133-144., 10Davies C, Troy GC. Deep mycotic infections in cats. J Am Anim Hosp Assoc 1996;32:380-391.]. Likewise, some studies have shown as slight male predilection while others have not [5Trivedi SR, Sykes JE, Cannon MS, et al. Clinical features and epidemiology of cryptococcosis in cats and dogs in California: 93 cases (1988-2010). J Am Vet Med Assoc 2011;239:357-369., 6Gerds-Grogan S, Dayrell-Hart B. Feline cryptococcosis: a retrospective evaluation. J Am Anim Hosp Assoc 1997;33:118-122., 8O’Brien CR, Krockenberger MB, Martin P, et al. Long-term outcome of therapy for 59 cats and 11 dogs with cryptococcosis. Aust Vet J 2006;84:384-392., 9Malik R, Wigney DI, Muir DB, et al. Cryptococcosis in cats: clinical and mycological assessment of 29 cases and evaluation of treatment using orally administered fluconazole. J Med Vet Mycol 1992;30:133-144., 10Davies C, Troy GC. Deep mycotic infections in cats. J Am Anim Hosp Assoc 1996;32:380-391.]. Staffordshire bull terriers, English bulldogs, Dalmatians, Irish setters, and Cocker spaniels have been overrepresented in certain studies [5Trivedi SR, Sykes JE, Cannon MS, et al. Clinical features and epidemiology of cryptococcosis in cats and dogs in California: 93 cases (1988-2010). J Am Vet Med Assoc 2011;239:357-369., 7McGill S, Malik R, Saul N, et al. Cryptococcosis in domestic animals in Western Australia: a retrospective study from 1995-2006. Medical mycology 2009;47:625-639.]. There is no sex predilection in dogs. Seasonal trends have been inconsistent between studies and infections can occur in any season [7McGill S, Malik R, Saul N, et al. Cryptococcosis in domestic animals in Western Australia: a retrospective study from 1995-2006. Medical mycology 2009;47:625-639., 9Malik R, Wigney DI, Muir DB, et al. Cryptococcosis in cats: clinical and mycological assessment of 29 cases and evaluation of treatment using orally administered fluconazole. J Med Vet Mycol 1992;30:133-144.]. Cats with FIV or FeLV are not predisposed to cryptococcosis, and co-infection likely does not affect prognosis, but response to treatment might be slower [6Gerds-Grogan S, Dayrell-Hart B. Feline cryptococcosis: a retrospective evaluation. J Am Anim Hosp Assoc 1997;33:118-122., 7McGill S, Malik R, Saul N, et al. Cryptococcosis in domestic animals in Western Australia: a retrospective study from 1995-2006. Medical mycology 2009;47:625-639., 8O’Brien CR, Krockenberger MB, Martin P, et al. Long-term outcome of therapy for 59 cats and 11 dogs with cryptococcosis. Aust Vet J 2006;84:384-392., 11Lester SJ, Kowalewich NJ, Bartlett KH, et al. Clinicopathologic features of an unusual outbreak of cryptococcosis in dogs, cats, ferrets, and a bird: 38 cases (January to July 2003). J Am Vet Med Assoc 2004;225:1716-1722.]. Cats with concurrent FIV are more likely to be asymptomatic carriers of Cryptococcus.
Clinical Signs
Disease can be localized to the nasal cavity and sinuses, skin, or CNS. It can also be multi-systemic. The nasal cavity and sinuses are most common site of infection in cats. Disease localized to the nasal cavity is relatively less common in dogs [5Trivedi SR, Sykes JE, Cannon MS, et al. Clinical features and epidemiology of cryptococcosis in cats and dogs in California: 93 cases (1988-2010). J Am Vet Med Assoc 2011;239:357-369., 7McGill S, Malik R, Saul N, et al. Cryptococcosis in domestic animals in Western Australia: a retrospective study from 1995-2006. Medical mycology 2009;47:625-639.]. Facial deformity, most common over the bridge of the nose, occurs due to sub-cutaneous or cutaneous lesions (Figure 1). These lesions might be ulcerated or have draining tracts. In some cases, a mass can be visualized extending through the nares. Nasal signs also include nasal discharge (bilateral or unilateral), stertor, and sneezing. Nasal obstruction can lead to open mouth breathing. Nasopharyngeal lesions can cause stridor, dysphagia and dyspnea [12Livet V, Javard R, Alexander K, et al. Cryptococcal nasopharyngeal polypoid mass in a cat. JFMS Open Rep 2015;1:2055116915597238.]. Local lymph nodes might be involved. Disease might spread from the nasal cavity into the brain and orbit. Ocular disease is relatively common and includes chorioretinitis, anterior uveitis, detached retinas and optic neuritis [5Trivedi SR, Sykes JE, Cannon MS, et al. Clinical features and epidemiology of cryptococcosis in cats and dogs in California: 93 cases (1988-2010). J Am Vet Med Assoc 2011;239:357-369.].

Figure 1: Sub-cutaneous swelling over the bridge of the nose in a cat with sinonasal cryptococcosis
There is overlap of clinical findings with sinonasal cryptococcosis and nasal neoplasia. Cats with nasal neoplasia tend to be older (median 9 years vs 6.5 years) [13Demko JL, Cohn LA. Chronic nasal discharge in cats: 75 cases (1993- 2004). J Am Vet Med Assoc 2007;230:1032-1037.]. Although less common, other fungi such as Histoplasma or Aspergillus can cause sinonasal disease, which can have clinical findings very similar to cryptococcosis. Other diseases that should be considered for chronic nasal disease include lymphoplasmacytic rhinitis, nasal foreign body, tooth root abscess, and nasopharyngeal polyp. Facial deformity, lymphadenopathy, and ocular or multisystemic disease would be less common, as compared with cryptococcosis, for all of these.
Skin lesions, most common on the head and neck, might be found anywhere on the body. Disease can be localized to the skin. CNS signs are reported in 6-55% of cats and 19-80% of dogs with cryptococcosis [5Trivedi SR, Sykes JE, Cannon MS, et al. Clinical features and epidemiology of cryptococcosis in cats and dogs in California: 93 cases (1988-2010). J Am Vet Med Assoc 2011;239:357-369., 7McGill S, Malik R, Saul N, et al. Cryptococcosis in domestic animals in Western Australia: a retrospective study from 1995-2006. Medical mycology 2009;47:625-639., 8O’Brien CR, Krockenberger MB, Martin P, et al. Long-term outcome of therapy for 59 cats and 11 dogs with cryptococcosis. Aust Vet J 2006;84:384-392., 11Lester SJ, Kowalewich NJ, Bartlett KH, et al. Clinicopathologic features of an unusual outbreak of cryptococcosis in dogs, cats, ferrets, and a bird: 38 cases (January to July 2003). J Am Vet Med Assoc 2004;225:1716-1722.]. Signs can be multifocal and localize to anywhere in the nervous system. Blindness, seizures, muscle tremors and twitching, mentation changes, ataxia, circling, cranial nerve deficits, and hyperesthesia and pain are the most common signs of neurologic disease [14Sykes JE, Sturges BK, Cannon MS, et al. Clinical signs, imaging features, neuropathology, and outcome in cats and dogs with central nervous system cryptococcosis from California. J Vet Intern Med 2010;24:1427-1438., 15Duncan C, Stephen C, Campbell J. Clinical characteristics and predictors of mortality for Cryptococcus gattii infection in dogs and cats of southwestern British Columbia. Can Vet J 2006;47:993-998.]. Dogs tend to have cervical pain in contrast to cats that more commonly have generalized or hind limb pain [14Sykes JE, Sturges BK, Cannon MS, et al. Clinical signs, imaging features, neuropathology, and outcome in cats and dogs with central nervous system cryptococcosis from California. J Vet Intern Med 2010;24:1427-1438.].
Cryptococcosis less commonly affects the lungs in cats and dogs as compared with other common invasive fungal infections (histoplasmosis, blastomycosis, coccidioidomycosis) [5Trivedi SR, Sykes JE, Cannon MS, et al. Clinical features and epidemiology of cryptococcosis in cats and dogs in California: 93 cases (1988-2010). J Am Vet Med Assoc 2011;239:357-369., 7McGill S, Malik R, Saul N, et al. Cryptococcosis in domestic animals in Western Australia: a retrospective study from 1995-2006. Medical mycology 2009;47:625-639.]. Likewise, coughing, tachypnea, and dyspnea are less common [5Trivedi SR, Sykes JE, Cannon MS, et al. Clinical features and epidemiology of cryptococcosis in cats and dogs in California: 93 cases (1988-2010). J Am Vet Med Assoc 2011;239:357-369.]. Lung involvement is more common in horses [7McGill S, Malik R, Saul N, et al. Cryptococcosis in domestic animals in Western Australia: a retrospective study from 1995-2006. Medical mycology 2009;47:625-639.]. Abdominal visceral organ involvement is uncommon, but is relatively more common in dogs as compared with cats [5Trivedi SR, Sykes JE, Cannon MS, et al. Clinical features and epidemiology of cryptococcosis in cats and dogs in California: 93 cases (1988-2010). J Am Vet Med Assoc 2011;239:357-369., 8O’Brien CR, Krockenberger MB, Martin P, et al. Long-term outcome of therapy for 59 cats and 11 dogs with cryptococcosis. Aust Vet J 2006;84:384-392.]. Any organ can be involved including pancreas, liver, kidney, urinary bladder, prostate, and adrenal gland [5Trivedi SR, Sykes JE, Cannon MS, et al. Clinical features and epidemiology of cryptococcosis in cats and dogs in California: 93 cases (1988-2010). J Am Vet Med Assoc 2011;239:357-369.]. Occasionally dogs will have disease localized to the GI tract which is believed to be due to ingestion of Cryptococcus [3Malik R, Hunt GB, Bellenger CR, et al. Intra-abdominal cryptococcosis in two dogs. J Small Anim Pract 1999;40:387-391., 16de Abreu DPB, Machado CH, Makita MT, et al. Intestinal Lesion in a Dog Due to Cryptococcus gattii Type VGII and Review of Published Cases of Canine Gastrointestinal Cryptococcosis. Mycopathologia 2017;182:597- 602.]. In general dogs, are less likely to have sinonasal and skin involvement and more likely to have disseminated disease and CNS involvement [5Trivedi SR, Sykes JE, Cannon MS, et al. Clinical features and epidemiology of cryptococcosis in cats and dogs in California: 93 cases (1988-2010). J Am Vet Med Assoc 2011;239:357-369., 7McGill S, Malik R, Saul N, et al. Cryptococcosis in domestic animals in Western Australia: a retrospective study from 1995-2006. Medical mycology 2009;47:625-639., 8O’Brien CR, Krockenberger MB, Martin P, et al. Long-term outcome of therapy for 59 cats and 11 dogs with cryptococcosis. Aust Vet J 2006;84:384-392.]. Other less common manifestations of cryptococcosis can include bone and joint disease, otitis media, and pyothorax [17Tisdall PL, Martin P, Malik R. Cryptic disease in a cat with painful and swollen hocks: an exercise in diagnostic reasoning and clinical decisionmaking. J Feline Med Surg 2007;9:418-423., 18Barrs VR, Allan GS, Martin P, et al. Feline pyothorax: a retrospective study of 27 cases in Australia. J Feline Med Surg 2005;7:211-222., 19Paulin J, Morshed M, Armien AG. Otitis interna induced by Cryptococcus neoformans var. grubii in a cat. Vet Pathol 2013;50:260-263., 20Siak MK, Paul A, Drees R, et al. Otogenic meningoencephalomyelitis due to Cryptococcus gattii (VGII) infection in a cat from Western Australia. JFMS Open Rep 2015;1:2055116915585022.].
Diagnosis
Clinically the diagnosis is often made by combination of supportive clinical findings and the cryptococcal antigen latex agglutination test. This test is highly sensitive (>95%) and specific (>95%) for the diagnosis of cryptococcosis [21Medleau L, Marks MA, Brown J, et al. Clinical evaluation of a cryptococcal antigen latex agglutination test for diagnosis of cryptococcosis in cats. J Am Vet Med Assoc 1990;196:1470-1473., 22Malik R, McPetrie R, Wigney DI, et al. A latex cryptococcal antigen agglutination test for diagnosis and monitoring of therapy for cryptococcosis. Aust Vet J 1996;74:358-364.]. Serum is most often tested but other body fluids such as CSF and cavitary effusions can be tested. Dogs and cats with cryptococcosis often have very high titers, but even a titer of 1:2 can be significant. It is recommended to confirm the diagnosis by other means, if possible, when titers are ≤1:200, because titers of this magnitude have been reported in a cat without proven cryptococcosis [5Trivedi SR, Sykes JE, Cannon MS, et al. Clinical features and epidemiology of cryptococcosis in cats and dogs in California: 93 cases (1988-2010). J Am Vet Med Assoc 2011;239:357-369.]. The antigen titer decreases with successful treatment and should be used for treatment monitoring (see below). Antigen detection by lateral flow has been described [23Reagan KL, McHardy I, Thompson GR, 3rd, et al. Evaluation of the clinical performance of 2 point-of-care cryptococcal antigen tests in dogs and cats. J Vet Intern Med 2019;33:2082-2089.]. As a point-of-care test it has a rapid turn-around time, with a lower diagnostic accuracy. The lateral flow test misclassified 7/101 animals as compared with the latex agglutination [23Reagan KL, McHardy I, Thompson GR, 3rd, et al. Evaluation of the clinical performance of 2 point-of-care cryptococcal antigen tests in dogs and cats. J Vet Intern Med 2019;33:2082-2089.]. PCR tests are commercially available for Cryptococcus, although the diagnostic performance of these remains unknown. MiraVista Diagnostics offers a cryptococcal antigen latex agglutination test (test code 319). It only requires 0.25 ml of serum or CSF.
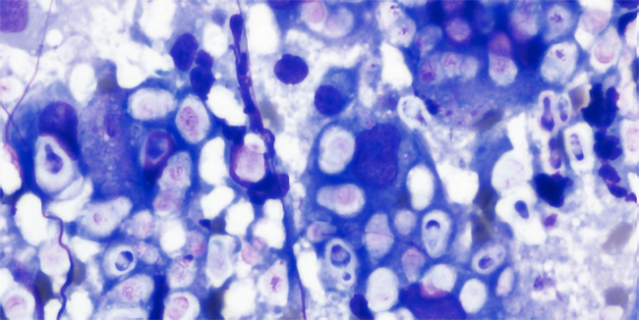
While Cryptococcus in the environment is found in many different forms, in the body Cryptococcus converts to a yeast, generally with a large polysaccharide capsule. Capsule deficient forms have been described. The yeasts reproduce by budding. Characteristic narrow budding yeasts found in tissue or body fluid samples can help make the diagnosis of cryptococcosis. Yeasts might be found in tissue aspirates, urine, CSF, cavitary effusions, skin swabs, nasal swabs, and sub-conjunctival aspirates, just to name a few. Cryptococcus is relatively easy to culture, and most studies report a relatively high positive culture rate when known infected tissues or body fluids are sampled [5Trivedi SR, Sykes JE, Cannon MS, et al. Clinical features and epidemiology of cryptococcosis in cats and dogs in California: 93 cases (1988-2010). J Am Vet Med Assoc 2011;239:357-369., 9Malik R, Wigney DI, Muir DB, et al. Cryptococcosis in cats: clinical and mycological assessment of 29 cases and evaluation of treatment using orally administered fluconazole. J Med Vet Mycol 1992;30:133-144.]. Positive cultures require at least 1 week of growth. C. neoformans can be differentiated from C. gattii by growth on L-canavanineglycine-bromthymol blue agar.
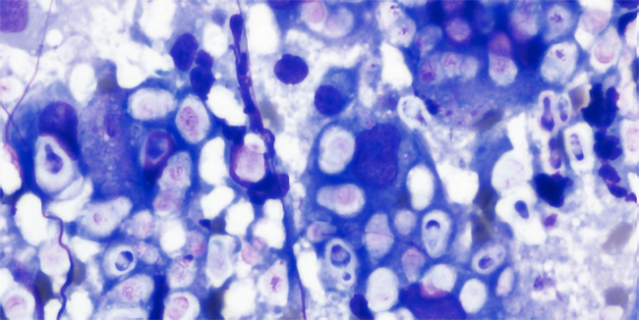
Figure 2: Cryptococcus yeast from a fine needle aspirate of a cutaneous facial mass in a cat. Note the narrow budding yeast and large clear capsule. Wright’s stain. Photo courtesy of Dr. Jim Meinkoth
Antifungal Treatment
The treatment of choice for life-threatening infection is amphotericin B. The older deoxycholate formulation has been used sub-cutaneously with some success [8O’Brien CR, Krockenberger MB, Martin P, et al. Long-term outcome of therapy for 59 cats and 11 dogs with cryptococcosis. Aust Vet J 2006;84:384-392.]. In some cases, flucytosine (5-FC) has been administered in addition to amphotericin B. Cats tolerate flucytosine better than dogs. Newer lipid or liposomal encapsulated formulations of amphotericin B (Abelcet® or Ambisome®) provide a decreased chance of nephrotoxicity and higher tolerable cumulative dose (Table 1). Fluconazole is the treatment of choice for mild to moderate disease and following amphotericin B treatment. Required treatment durations are long, generally at least 6 months. Occasionally, animals will require antifungal treatment life-long. Serum antigen titers decrease with successful treatment and should be measured every 2-3 months to monitor response [9Malik R, Wigney DI, Muir DB, et al. Cryptococcosis in cats: clinical and mycological assessment of 29 cases and evaluation of treatment using orally administered fluconazole. J Med Vet Mycol 1992;30:133-144.]. Ideally antigen titers return to negative before antifungal treatment is discontinued. Occasionally when all other clinical indicators suggest disease remission antifungal treatment can be discontinued with a low positive titer (1:2) with close monitoring. The following criteria should be met before discontinuing treatment.
- Resolution of clinical signs
- Resolution of imaging abnormalities (or static minimal disease)
- Serum antigen negative (latex agglutination test)
Disease relapse is always possible and has been reported in about 16-17% of cases [8O’Brien CR, Krockenberger MB, Martin P, et al. Long-term outcome of therapy for 59 cats and 11 dogs with cryptococcosis. Aust Vet J 2006;84:384-392., 9Malik R, Wigney DI, Muir DB, et al. Cryptococcosis in cats: clinical and mycological assessment of 29 cases and evaluation of treatment using orally administered fluconazole. J Med Vet Mycol 1992;30:133-144.]. An increase in antigen titer after discontinuation of antifungal therapy is suggestive of disease relapse. Serum antigen titers (latex agglutination test) should be measured at 3 months and then every 6 -12 months after discontinuing antifungal therapy to assist with early detection of disease relapse.
Antifungal resistant strains of Cryptococcus have been reported. In general, the antifungal sensitivity of C. gattii is less predictable as compared with C. neoformans [24Singer LM, Meyer W, Firacative C, et al. Antifungal drug susceptibility and phylogenetic diversity among Cryptococcus isolates from dogs and cats in North America. J Clin Microbiol 2014;52:2061-2070.]. Itraconazole is also effective against Cryptococcus and can be used if fluconazole is not well tolerated or if inadequate response. For animals that do not respond to fluconazole or itraconazole (salvage therapy), voriconazole or posaconazole might be treatment options (Table 1).
Additional Treatments
Seizures should be treated aggressively. Status epilepticus should be treated with midazolam or diazepam. Additional anti-seizure medications will be needed for longer term control which might include phenobarbital, levetiracetam, zonisamide, and KBr (dogs only). Likewise, intracranial hypertension should be treated aggressively with mannitol or hypertonic saline. Indications of intracranial hypertension might include systemic hypertension with bradycardia and progressive neurologic dysfunction. Analgesia might be required, especially for bone or CNS involvement. Other supportive care such as IV fluids, nutritional support, and anti-nausea medications, just to name a few, might be needed on a case-by-case basis.
Prognosis
Even with antifungal treatment the prognosis is guarded. Reported survival rates are 45-76% in cats and 27-71% in dogs [7McGill S, Malik R, Saul N, et al. Cryptococcosis in domestic animals in Western Australia: a retrospective study from 1995-2006. Medical mycology 2009;47:625-639., 8O’Brien CR, Krockenberger MB, Martin P, et al. Long-term outcome of therapy for 59 cats and 11 dogs with cryptococcosis. Aust Vet J 2006;84:384-392., 15Duncan C, Stephen C, Campbell J. Clinical characteristics and predictors of mortality for Cryptococcus gattii infection in dogs and cats of southwestern British Columbia. Can Vet J 2006;47:993-998.]. CNS involvement is a negative prognostic indicator and animals with CNS involvement are 4 times as likely to die from infection [7McGill S, Malik R, Saul N, et al. Cryptococcosis in domestic animals in Western Australia: a retrospective study from 1995-2006. Medical mycology 2009;47:625-639., 8O’Brien CR, Krockenberger MB, Martin P, et al. Long-term outcome of therapy for 59 cats and 11 dogs with cryptococcosis. Aust Vet J 2006;84:384-392., 15Duncan C, Stephen C, Campbell J. Clinical characteristics and predictors of mortality for Cryptococcus gattii infection in dogs and cats of southwestern British Columbia. Can Vet J 2006;47:993-998.]. Altered mentation appears to be an especially important prognostic indicator [14Sykes JE, Sturges BK, Cannon MS, et al. Clinical signs, imaging features, neuropathology, and outcome in cats and dogs with central nervous system cryptococcosis from California. J Vet Intern Med 2010;24:1427-1438.]. Disseminated disease, as compared with localized disease, was also a negative prognostic indicator in 1 study [7McGill S, Malik R, Saul N, et al. Cryptococcosis in domestic animals in Western Australia: a retrospective study from 1995-2006. Medical mycology 2009;47:625-639.].
Table 1. Treatment recommendations for dogs and cats with cryptococcosis
| Category |
Dose |
Duration |
Mild-Moderate
First choice |
Fluconazole 20 mg/kg/day 6-12 months |
6-12 months |
Mild-Moderate
Second choice |
Itraconazole 10 mg/kg/day for 3 days then 5 mg/kg/day (dog)
Itraconazole 10 mg/kg/day (capsule cat)
Itraconazole 4-7 mg/kg/day (solution cat) |
6-12 months |
| Severe disease*$^ |
Amphotericin B 0.5-1.0 mg/kg (cat) or 1.0-1.5 mg/kg (dog) IV 3 times a week or EOD |
Up to 24 mg/kg (dog) or 12 mg/kg (cat) cumulative dose |
| Fluconazole (as above) |
6-12 months |
| Salvage therapy |
Posaconazole ER 5 mg/kg EOD (dog)
Posaconazole 8-10 mg/kg/day (dog and cat)
Voriconazole 5 mg/kg BID (dog)
Voriconazole 12.5 mg (total dose) q 72 h(cat) |
>6 months |
* Lipid or liposomal amphotericin B. Follow with fluconazole therapy.
$ Flucytosine might be synergistic with amphotericin B and can be given with CNS signs (cats not dogs).
^ Higher doses might be well tolerated in dogs – up to 3 mg/kg (dog).
REFERENCES:
- Emmons CW. Saprophytic sources of Cryptococcus neoformans associated with the pigeon (Columba livia). American journal of hygiene 1955;62:227-232.
- Duncan CG, Stephen C, Campbell J. Evaluation of risk factors for Cryptococcus gattii infection in dogs and cats. J Am Vet Med Assoc 2006;228:377-382.
- Malik R, Hunt GB, Bellenger CR, et al. Intra-abdominal cryptococcosis in two dogs. J Small Anim Pract 1999;40:387-391.
- Medleau L, Hall EJ, Goldschmidt MH, et al. Cutaneous cryptococcosis in three cats. J Am Vet Med Assoc 1985;187:169-170.
- Trivedi SR, Sykes JE, Cannon MS, et al. Clinical features and epidemiology of cryptococcosis in cats and dogs in California: 93 cases (1988-2010). J Am Vet Med Assoc 2011;239:357-369.
- Gerds-Grogan S, Dayrell-Hart B. Feline cryptococcosis: a retrospective evaluation. J Am Anim Hosp Assoc 1997;33:118-122.
- McGill S, Malik R, Saul N, et al. Cryptococcosis in domestic animals in Western Australia: a retrospective study from 1995-2006. Medical mycology 2009;47:625-639.
- O’Brien CR, Krockenberger MB, Martin P, et al. Long-term outcome of therapy for 59 cats and 11 dogs with cryptococcosis. Aust Vet J 2006;84:384-392.
- Malik R, Wigney DI, Muir DB, et al. Cryptococcosis in cats: clinical and mycological assessment of 29 cases and evaluation of treatment using orally administered fluconazole. J Med Vet Mycol 1992;30:133-144.
- Davies C, Troy GC. Deep mycotic infections in cats. J Am Anim Hosp Assoc 1996;32:380-391.
- Lester SJ, Kowalewich NJ, Bartlett KH, et al. Clinicopathologic features of an unusual outbreak of cryptococcosis in dogs, cats, ferrets, and a bird: 38 cases (January to July 2003). J Am Vet Med Assoc 2004;225:1716-1722.
- Livet V, Javard R, Alexander K, et al. Cryptococcal nasopharyngeal polypoid mass in a cat. JFMS Open Rep 2015;1:2055116915597238.
- Demko JL, Cohn LA. Chronic nasal discharge in cats: 75 cases (1993- 2004). J Am Vet Med Assoc 2007;230:1032-1037.
- Sykes JE, Sturges BK, Cannon MS, et al. Clinical signs, imaging features, neuropathology, and outcome in cats and dogs with central nervous system cryptococcosis from California. J Vet Intern Med 2010;24:1427-1438.
- Duncan C, Stephen C, Campbell J. Clinical characteristics and predictors of mortality for Cryptococcus gattii infection in dogs and cats of southwestern British Columbia. Can Vet J 2006;47:993-998.
- de Abreu DPB, Machado CH, Makita MT, et al. Intestinal Lesion in a Dog Due to Cryptococcus gattii Type VGII and Review of Published Cases of Canine Gastrointestinal Cryptococcosis. Mycopathologia 2017;182:597- 602.
- Tisdall PL, Martin P, Malik R. Cryptic disease in a cat with painful and swollen hocks: an exercise in diagnostic reasoning and clinical decisionmaking. J Feline Med Surg 2007;9:418-423.
- Barrs VR, Allan GS, Martin P, et al. Feline pyothorax: a retrospective study of 27 cases in Australia. J Feline Med Surg 2005;7:211-222.
- Paulin J, Morshed M, Armien AG. Otitis interna induced by Cryptococcus neoformans var. grubii in a cat. Vet Pathol 2013;50:260-263.
- Siak MK, Paul A, Drees R, et al. Otogenic meningoencephalomyelitis due to Cryptococcus gattii (VGII) infection in a cat from Western Australia. JFMS Open Rep 2015;1:2055116915585022.
- Medleau L, Marks MA, Brown J, et al. Clinical evaluation of a cryptococcal antigen latex agglutination test for diagnosis of cryptococcosis in cats. J Am Vet Med Assoc 1990;196:1470-1473.
- Malik R, McPetrie R, Wigney DI, et al. A latex cryptococcal antigen agglutination test for diagnosis and monitoring of therapy for cryptococcosis. Aust Vet J 1996;74:358-364.
- Reagan KL, McHardy I, Thompson GR, 3rd, et al. Evaluation of the clinical performance of 2 point-of-care cryptococcal antigen tests in dogs and cats. J Vet Intern Med 2019;33:2082-2089.
- Singer LM, Meyer W, Firacative C, et al. Antifungal drug susceptibility and phylogenetic diversity among Cryptococcus isolates from dogs and cats in North America. J Clin Microbiol 2014;52:2061-2070.